CONTRACEPTION
From adolescence to menopause, follow-up is essential.
It provides contraception, replacement therapy and cancer screening.
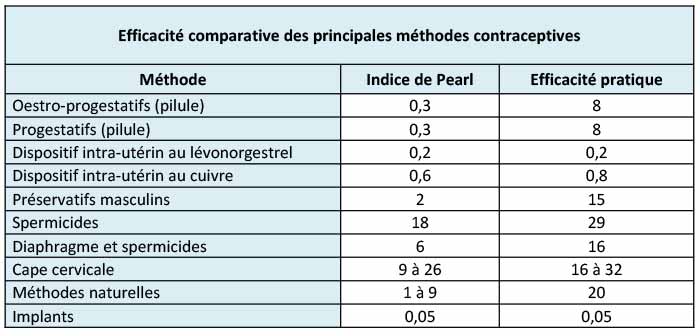
The effectiveness of the various contraceptive methods is measured using the Pearl Index. The theoretical index is based on the number of (unplanned) pregnancies that occur for each contraceptive method if used by 100 women for one year. For example, a Pearl Index of 2 indicates that in one year, 2 women out of 100 using the contraceptive method in question fell pregnant. We have to distinguish theoretical effectiveness (which presupposes correct usage of the contraceptive method) from practical effectiveness (which also reflects, for example, instances of forgotten pills or the incorrect use of a condom).
As you can see in the table above, the safest option is the implant or the hormonal coil (IUD = intrauterine device). However, conventional methods of contraception (oestro-progestative or progestative) are also very effective, much more so than so-called ‘natural’ methods – but their effectiveness depends on proper and everyday use…
1- Oral contraception: ‘the pill’
There are two types of contraceptive pill: the combined pill (oestro-progestative) and the progestogen-only pill.
It works by blocking ovulation, thickening the cervical mucus (the sticky substance produced in the neck of the uterus), and affecting the endometrium (lining of the womb). There is a big choice of combined pills that are classified by ‘generations’. Regarding the progestogen-only pills, we talk about micro- or macroprogestatives depending on the dosage. You will notice that certain pills come in strips of 21, and others of 28 days – this depends on the type of contraceptive.
Your pill is chosen by your gynaecologist, who takes into account your medical background and your expectations. The contraceptive pill is the most frequently prescribed means of contraception and is very effective if it is taken strictly on a daily basis. However, it is not a good option if you have problems with absorbing food (malabsorption), frequent vomiting or diarrhoea, or if you are simply too absent-minded to regularly take daily medication.
The side effects of the pill do not necessarily occur in each case but may include: nausea, painful breasts, mood swings, water retention, pelvic pain and changes in libido… These symptoms typically improve after two to three months. If such problems persist, you should consult your doctor to consider a different type of contraception and exclude the risk of another cause for the symptoms. It’s important to understand that these symptoms are not always associated with the pill.
The pill, whichever type it is, is efficient as a contraceptive, but it may also have beneficial effects in the case of premenstrual syndrome, menorrhagia (abnormally heavy bleeding at menstruation), functional ovarian cysts or the acne. The pill is therefore sometimes not prescribed at all for
contraceptive reasons.
2- Transdermal contraceptive patch
This is a combined contraceptive method containing both oestrogen and progesterone that is applied weekly. There is a lower chance of forgetting about it, and a lower risk of malabsorption as, in this case, hormone absorption happens through the skin.
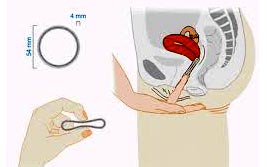
3- The contraceptive ring
This is a flexible plastic ring that has to be inserted at the bottom of the vagina, and that diffuses oestrogen and progesterone hormones through the vaginal wall. It remains in place for 3 weeks followed by a break of one week corresponding to the period of menstruation. It is placed and removed easily, in the same way as vaginal tampons.
4- Contraceptive injection
This is a long-acting reversible contraceptive (LARC) based on progesterone. It is an intramuscular injection (meaning that it is injected into the muscles) that is given every 3 months. This is an invisible and discreet method. However, it requires more frequent consultations.
5- The implant
This match-sized flexible (progesterone-only) tube is placed in the arm under local anaesthetic, during a normal gynaecological visit. It is effective for three years. The implant is the most effective method of contraception. It may reduce or even totally stop the periods, but women may also experience light irregular bleeding in between, that may be annoying in everyday life. An implant is, therefore, an interesting option when there are contraindications against oestrogen; if the patient is less disciplined to take regular medication or if there is a problem of malabsorption, for example.
6- The coil: the intrauterine device (IUD)
This is a small, T-shaped object inserted into the uterus (the womb), intended to stay there for 3-5 years. There are two kinds of IUDs. One of them is the copper coil that inactivates the sperm and
prevents the nidation (the embedding of a fertilised egg cell). In this case, the period still occurs, and it is often more abundant.
The other kind of IUD is a hormonal coil (containing progestin). This makes the endometrium thinner and the cervical mucus thicker. (‘Endometrium’ means the slimy layer of cells lining the
womb; ‘cervical mucus’ is the sticky substance produced in the neck of the womb). As a consequence, the period may become weaker, or it may even disappear. The hormonal IUD has
a higher efficiency than the copper one.
The IUD in placed during a normal gynaecological visit, when the period makes the insertion easier. For a better comfort, it is recommended to take a painkiller one hour before the installation of the IUD. Six weeks later, an ultrasound control has to be done to ensure the correct positioning of the IUD.
Nearly a third of patients are pleasantly surprised by the hormonal coil and enjoy seamless contraception for five years without having their period and without unpleasant symptoms. However, a small proportion of patients report periods of irregular bleeding, pelvic pain, ovarian cysts or systemic hormonal effects such as headaches, acne, weight gain or even mood disorders.
7- Condoms
Condoms are less effective than all other methods of contraception previously mentioned. However, their use is very important for protection against sexually transmitted diseases, and they are the only methods of contraception which is effective for this. Be careful! The so-called ‘natural’ methods are not reliable.
8- Sterilisation
Sterilisation is a surgical procedure most often carried out by laparoscopy (by inserting a small viewing tube [laparoscope] through the abdominal wall to view the organs and permit small-scale surgery). Sterilisation provides permanent contraception. The most common types of sterilisation procedures are ‘tubal ligation’ or ‘bilateral salpingectomy‘ (for women) and ‘vasectomy’ (for men). This option can be considered when you decide, after thorough reflection, that you do not want fall pregnant in the future, and in agreement with your gynaecologist. It is important to make sure that you have considered all other methods of contraception before undergoing such a procedure. In Luxembourg, the cost of the sterilisation procedure is not refunded by CNS.
During the consultation, your gynaecologist will ask you to fill out an extensive questionnaire and examine you thoroughly to ensure that there are no contraindications before s/he prescribes you any contraceptives.
The main and ‘absolute’ contraindications are:
– Arterial and/or venous thromboembolic incident in the personal medical history
– Severe or poorly regulated arterial hypertension (high blood pressure)
– Breast cancer in the personal medical history
– Valvular heart disease, congestive heart failure
– Long-standing diabetes
– Severe hepatobiliary diseases: hepatitis (jaundice), cirrhosis (liver disease) and hepatic adenoma (an uncommon benign liver tumour that is hormone induced)
– Non-diagnosed pregnancies and genital bleeding
‘Relative’ contraindications are among others: smoking, obesity (being overweight), etc.…
It is a last-minute method of contraception that can be used following sexual intercourse without or with unsatisfactory protection: when no contraceptive method was used, when the condom broke, when you forgot to take the contraceptive pill, if you vomited or had diarrhoea after taking the tablet, if the patch peeled off, etc.
It is less effective than a regular method, but the sooner it is taken after intercourse, the more effective it is.
It comes in the form of a single pill. It must be taken as soon as possible because its effectiveness decreases with time. There are 2 types of pill:
A pill containing levonorgestrel, which can be taken up to 72 hours (3 days) after sexual intercourse without or with unsatisfactory protection.
Or a pill containing ulipristal acetate, which can be taken up to 120 hours (5 days) after sexual intercourse without or with unsatisfactory protection.
After taking the pill, some women experience mild side effects such as nausea, headaches, abdominal pain, dizziness or a mild loss of blood, but these usually disappear within 48 hours. The period may also come early or late.
On the other hand, there is no risk of sterility, nor an increased risk of spontaneous miscarriage or extrauterine pregnancy.
Oral contraceptives are not associated with an increased risk of cancer. Moreover, it was found that the risk of colo-rectal, uterine and ovarian cancer among pill users was lower than among pill non-users. Concerning breast cancer, studies differ to an extent, but it seems that there is a slightly increased risk linked to the combined pill. At the same time, there is a contraindication to hormonal contraceptives if the patient has had breast cancer in her personal medical history.
Puberty: For a long time, oral hormonal contraception has been the chosen method. Currently, however, there are more and more different means being made available to young patients in order to best adapt to their rhythm of life. In the case of repeated problems with regular pill-taking, or teenagers, by whom there is a high risk of running into such problems, the implant, the patch or the vaginal ring can be considered as an interesting solution.
The IUD can be used by teenagers, but its use is limited given the higher risk of infections and the difficulties of insertion related to nullparity (the fact that they have never given birth yet). However, there is a more recently developed IUD especially designed for young women who have not yet had a pregnancy.
After the age of 35-40: Smoking, body weight, the condition of the cardiovascular system and the breasts must be taken into account. Macroprogestins have their place here. Hormonal IUDs are available for those (not few at all) who have menorrhagia or who do not want to think too much about contraception anymore. For those with no risk factor, the pill is still an important method.
Postnatal period (right after giving birth): It is often recommended for new mothers to take a microprogestin pill (Cerazette) from the 10th day after giving birth. From the postnatal check-up taking place two months after giving birth, any method can be considered once breastfeeding has been stopped.
The morning-after pill is solely an emergency solution.