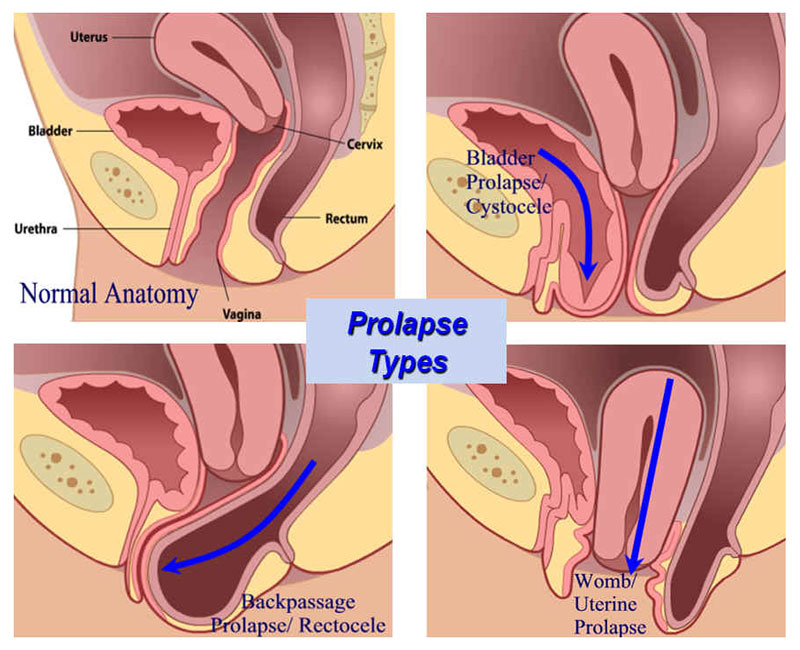
The organs within the small pelvis of women are maintained through a set of muscles and ligaments that constitute the pelvic floor. The latter functions like a hammock on which the bladder, the uterus (the womb) and the rectum (the final section of the large intestine) rest. We talk about a ‘prolapse’ (or commonly speaking: ‘the descent of an organ’) when these organs are no longer sustained and protrude either in the vagina to different degrees or even beyond the vulva when the prolapse is externalised. It may concern the bladder (in this case, the anomaly is called cystocele), the uterus (hysteroptosis) and the rectum (rectocele) separately or together.
So, the treatment will depend on the type of the prolapse and its degree of seriousness, while the age of the patient and the antecedents will naturally also be taken into account. To provide the best treatment possible, most often, it is necessary to make a complete preoperative assessment:
- A pelvic ultrasound
- A urodynamic assessment to see if there is associated urinary incontinence
- And sometimes also a colpocystogramme (dynamic radiography of the pelvic organs)
Prolapse is responsible for a set of various symptoms. It may cause pelvic heaviness or a ball-like protrusion outside the vulva, or it may lead to urinary, sexual or digestive symptoms.
The intervention that your gynaecologist proposes is a surgery with the aim of correctly repositioning the bladder, the vagina and rectum in the small pelvis.
This repositioning is often accompanied by strengthening the means that provide support to these organs by using synthetic reinforcing tissue (a prosthetic implant) that is compatible with the human body.
Finally, an intervention may be carried to complete the treatment of stress urinary incontinence.
Depending on your medical profile, it may be necessary to remove the uterus (in whole or in part), and/or the ovaries. This has to be discussed with your surgeon.
Rehabilitation is possible, but it is only effective when the prolapse is not significant. Using a pessary can be a solution: this is a device to be placed in the vagina, designed to contain the prolapse. It is often used when an intervention cannot be carried out as quickly as would be desirable. It may be worn temporarily or permanently.
The intervention can be carried out according to different tracks (abdominal or vaginal) and by different techniques. Your surgeon will explain you your possibilities. To treat your prolapse is not of vital importance. However, if it is not treated, the prolapse will get worse up to the point of externalisation. Further consequences may include urinary retention (blockage of the emptying of the bladder), a dilation of the kidneys with renal impairment, and ulceration of the vagina and the cervix (the neck of the womb). Nevertheless, these complications are rare, and it is rather the discomfort caused by the
prolapse that will probably motivate your decision to have an operation.
Abdominal track: Promontofixation
The intervention is carried out under general anaesthetic. It can be done by laparoscopy (a type of surgical procedure in which a small incision is made, through which a viewing tube (laparoscope) is inserted to view the organs in the abdomen or permit small-scale surgery), or by abdominal incision. During the operation, the patient is lying on the back. A urinary catheter is put in place at the beginning of the intervention.
- A synthetic prosthesis is fixed between the bladder and the anterior (front) wall of the vagina.
- A second prosthesis may be fixed between the rectum and the posterior (back) wall of the vagina.
- The/each prosthesis is then attached to a very strong ligament located in front of the spinal column, in front of the sacrum bone, at the promontory.
The catheter is usually removed on the same day after the intervention. Intestinal transit normally resumes within 48 hours. However, patients usually experience constipation in the first month after the intervention. Therefore it is recommended to use a laxative during this period.Patients usually stay in the hospital for one day, and the convalescence can be expected to last for 1 month. During this time, one must restrain from abdominal efforts: it is not allowed to carry heavy loads or push strong when going to the toilet. However, you will be able to walk and drive. In any case, one must avoid strong efforts.
Vaginal track:
The interventions carried out through natural channels make it possible to avoid incisions and generally do not require the use of a prosthesis. The intervention is carried out under general or loco-regional anaesthetic (making either the whole or only a part of the body insensitive respectively). During the operation, the patient is in the gynaecological position. A urinary catheter is put in place at the beginning of the intervention.
An incision is performed in the anterior or posterior (front or back) wall of the vagina. The organs are released so that they can be repositioned correctly. For fixing the organs, the surgeon may use the patient’s ligaments or a synthetic tissue. In some cases, a hysterectomy (surgical removal of the womb) may be recommended. This intervention is also carried out by the vaginal track, and it can be required because of the severity of the prolapse of your uterus or a pathology (disease) of the latter. Your surgeon will explain to you if such an intervention is necessary. Patients usually stay in the hospital for 1-2 days, and the convalescence can be expected to last for 1 month. During this time, one must restrain from abdominal efforts: it is not allowed to carry heavy loads or push strong when going to the toilet.
However, you will be able to walk and drive. In any case, one must avoid strong efforts.
Surgery of stress urinary incontinence (SUI)
Urinary incontinence is an involuntary leakage of urine that causes discomfort. There are several types of urinary incontinence:
- Stress Urinary Incontinence (SUI): leakage occurs at the time of exerting force (by a sports activity, coughing, laughing, sneezing, walking, changing position, etc.).
- Urge Urinary Incontinence (UUI): it means that the need to urinate is (often) urgent and uncontrollable.
- Mixed Urinary Incontinence (MUI): it combines the symptoms of stress incontinence and urge incontinence.
The consequences:
- The weakness of the muscles of the perineum (part of the body at the bottom of the small pelvis where the ends of the urinary, the genital and the digestive track all cross) that are responsible for supporting the bladder and the urethra (the tube that carries urine out of your body).
- The weakness of the sphincter of the urethra (the muscle responsible for closing the bladder).
Woman are by default disadvantaged in this respect because their urethra is very short, their sphincter is not too powerful, and their perineum is weakened by the several holes allowing for the passage of the urethra, the vagina and the rectum. Their perineum is strained during the pregnancy and especially by giving birth.
Finally, the lack of hormones after the menopause leads to the tissues getting dryer and an additional vulnerability. If perineal rehabilitation fails or the stress incontinence is very significant, intervention is
currently one of the most effective ways to make SUI disappear on the long term. At the moment, there is no efficient medication to treat stress incontinence.
It consists of placing a small synthetic strip under the urethra. This strip will stay under the urethra like a hammock, supporting it at the time of exerting force to prevent leaks. Note that this intervention can not bring relief in the case of all types of urinary incontinence. Your doctor will decide if this technique is appropriate after having examined your case and carrying out a few complementary examinations, such as a urodynamic assessment.
During the operation that is carried out with the patient lying in the gynaecological position, a small incision of 2 cm is made inside the vagina. The strip is passed through this little hole and positioned under the urethra the using needles. Placement of a sub-urethral strip
The intervention takes 20-30 minutes.
Patients usually stay in the hospital for a couple of hours to up to 48 hours.
The intervention goes with little pain. The thighs may be painful for a few days afterwards.
This is because of the use of the needles during the operation.
The average convalescence period lasts for two weeks, but the time needed before taking up
work again may differ according to your profession. As soon as you leave the hospital, you can resume your normal activities, but you have to avoid strong efforts and carrying loads heavier than 5 kg for a month.
Urodynamic assessment
This examination measures pressure at different points and observes the flow of the urine during voiding, using small probes introduced into the bladder. It makes it possible to accurately analyse the functioning of the bladder and thus to choose the best the necessary treatment.
In some cases, medication is necessary to help when you have to pass urine too often, or to improve any incontinence of neurological origin.
We conduct this examination in our institute, and Dr Sanjurjo, our urologist specialised in this domain will be able to evaluate the results so that we can propose you the best possible treatment.