Hysterectomy is a surgical procedure in which the uterus (womb) is removed.
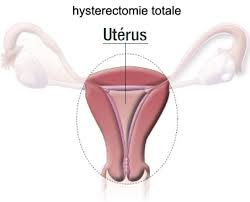
In a total hysterectomy we remove the cervix or neck of the uterus together with the body.
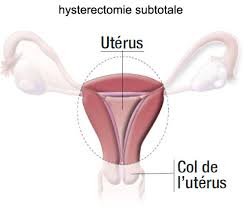
We call a hysterectomy subtotal if the neck is left in place.
During this intervention we have the option to remove or not the ovaries. The Fallopian tubes are commonly removed as well to reduce the risk of ovarian cancer. The ovaries can also be taken out.
Surgical techniques:
Surgery can be accomplished with different approaches:
1- Vaginal hysterectomy:
the uterus is removed through the vagina, so no abdominal incision is necessary. Anaesthesia can be spinal or general during this intervention.
During a pre-operative consultation your specialist can evaluate the feasibility of this approach depending on specific conditions.
2- Laparoscopic hysterectomy:
Surgery is performed by small incisions on the abdominal wall. The uterus is extracted through the natural pathway or cut into little pieces in the abdominal cavity and extracted through one of the little abdominal incisions.
For both types of interventions, 1 or 2 days of hospitalisation are required. A urinary catheter is placed during the intervention and removed soon after. The same day you can get out of bed, eat and walk.
The complete recovery takes one month.
3- Abdominal hysterectomy:
In certain cases the traditional approach with incision through the abdominal wall needs to be used, for example if the uterus is too big.
The incision is usually placed transversally, on the lower part of the abdomen, like for a Caesarean section.
After abdominal hysterectomy, a 4- to 5-day hospital stay is generally required, and you may experience more pain. A suitable pain killer protocol is applied, that may imply intravenous morphine derivatives.
Total recovery is achieved after one month as well.
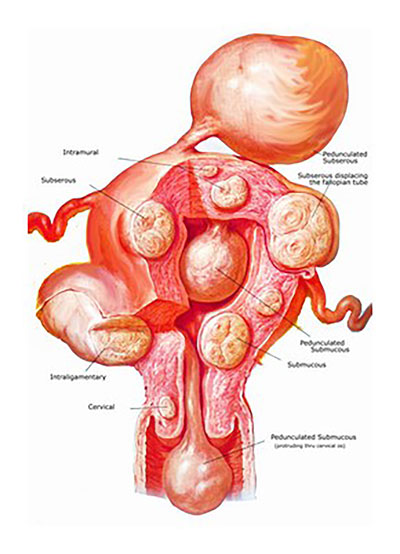
A myoma is a benign tumour of the uterine muscle.
It is a frequent condition that often affects women after the age of 40, but it can occur at earlier ages.
The presence of myomas is commonly not dangerous, but they can cause symptoms such as heavy menstrual bleeding, abdominal pain or frequent urge to urinate. In younger women they can be responsible for fertility problems because of their position or their effect on the vascularisation of the uterus. Ultrasound and MRI are the best imaging methods to visualise myomas, with MRI being more precise in the pre-operative period.
Myomectomy (surgical resection of myomas) may be indicated for different reasons. Most frequently this intervention is carried out by laparoscopy and the myomas are removed from the abdominal cavity through a little abdominal incision after having been cut into pieces .
The postoperative period consists of a maximum of two days of hospital stay and a full recovery after 2 to 4 weeks.
There is no difference between the two technics that would favour either method in view of a later pregnancy , so because of its more comfortable post-operative period, we recommend the laparoscopic approach.

1- Diagnostic hysteroscopy:
The aim is to visualise directly the mucosal layer of the uterus along with the tubal orifices. The procedure can be complemented by simultaneous biopsy (extraction of tissue for examination).
2- Interventional hysteroscopy:
During this type of surgery we can visualise and treat intra-uterine conditions at the same time. With general or loco-regional anaesthesia we introduce a bigger instrument to be able to cut and coagulate with the aim of removing myomas, polyps or the whole uterine mucosa.
Using the natural pathways enables a very quick recovery of the patient, no hospital stay is needed.
Conisation is the resection of a small part of the uterine cervix.
1- Indications :
This intervention is proposed in the case of cervical dysplasia (a pre-cancerous condition). In the case of low-grade dysplasia we can propose a regular follow-up, but in the case of high grade anomalies, surgical intervention is necessary.
Dysplasia is detected by a PAP test, but can only be diagnosed by a biopsy (tissue specimen) taken under colposcopy guidance.
If not treated, cervical dysplasia can progress to cervical cancer after a few years.
Conisation has two important objectives:
Diagnostic : it allows us to analyse and confirm the type of the lesion.
Therapy : with the resection of the suspicious zone, we remove all abnormal cells and thereby diminish the risk of development into cervical cancer.
2- The surgical technique:
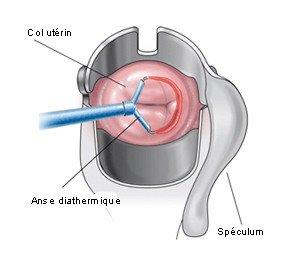
The suspicious zone is resected with a special electric wire within a few minutes.
The intervention is carried out in one day, no long recovery is needed.
3- Complications :
The postoperative period is generally very simple, but in certain cases complications can arise: bleeding can occur until 10 days after surgery. It is a normal healing process consisting of the breakdown of the scar crust. Sometimes a tamponade or compress may be necessary or in rare cases a new surgical intervention.
A long-term complication can be the stenosis of the cervical canal, requiring local dilation. The risk for a later pregnancy is very low, but an adapted follow-up is necessary.